Pancreatitis, an inflammation of the pancreas, is a fairly dangerous disease that significantly affects people's quality of life. And an important component of the correct treatment of this unpleasant disease is proper nutrition, which has a positive effect on the functioning of the organ. What should be the diet for pancreatitis? Read in our material.
Don't self-medicate! In our articles we collect the latest scientific data and opinions from authoritative experts in the field of health. But remember: only a doctor can make a diagnosis and prescribe treatment. We want to help those who are faced with diseases of the pancreas (by the way, among office workers and former students, pancreatitis is in third place "in popularity") and therefore we have compiled basic recommendations on nutrition for pancreatitis and cholecystitis in this article. We also have sample menusand prepared some useful recipes. Read it, it will be useful!
What is Pancreatitis?
Pancreatitis is an inflammation of the pancreas, which is involved in the digestive process and also regulates metabolism. This is a "2-in-1" organ, it has a complex structure: the bulk of the gland secretes the enzymes necessary for the digestion of food into the intestine, and the so-called "pancreatic islets" are an endocrine organ thatHormone insulin produced.
When the pancreas becomes inflamed, the release of enzymes into the duodenum stops. As a result, these aggressive substances are activated in the gland itself and begin to destroy it - this process is often called self-digestion. This releases toxins that can travel through the bloodstream to other organs and damage them. Pancreatitis can be acute or chronic.
Acute inflammation of the pancreas
Acute pancreatitis is a dangerous condition that requires immediate treatment, usually in hospital. Most commonly, it occurs due to alcohol abuse or gallstone disease, when a stone blocks the bile duct. The disease is characterized by severe pain in the upper abdomen, some of which radiates to the back; nausea; to throw up; general deterioration of condition.
Chronic pancreatitis
When the pancreas becomes chronically inflamed, the organ is gradually destroyed. The main causes of the disease are alcohol consumption and smoking. The most typical manifestation is abdominal pain, which usually occurs after eating. The lack of digestive secretion from the pancreas leads to poor digestion of food, bloating and bloating. There is often a lack of appetite and weight can decrease.
Symptoms of pancreatitis
The main symptom of both acute and chronic inflammation of the pancreas is pain in the upper abdomen. Such pain is often belt-shaped. In the chronic form, stomach problems, nausea and stool disorders are often observed. Unpleasant sensations lead to suspicion of pancreatitis, and then the diagnosis is confirmed using tests and other studies.
Why do you need a diet for pancreatitis (inflammation of the pancreas)?
The diet for pancreatitis in adults is designed to reduce the load on the affected organ so that it can recover. In acute pancreatitis, it is also important to reduce enzyme synthesis in order to stop the process of gland destruction.

Principles of nutrition for pancreatitis
- Refusal of any foods that stimulate the production of enzymes - smoked, spicy, pickled, fried.
- The food should be warm (not cold or hot) and mushy.
- Meals should be in portions and portions should be small.
- The focus of the diet is on protein products - up to 200 grams of which should be consumed per day. But fats and carbohydrates are significantly limited.
- The amount of salt is reduced to 3-5 grams, the dishes are not salted when cooking.
- Raw food is excluded. Fresh vegetables and fruit may not be consumed, only cooked or baked ones.
- Carbohydrates are consumed in moderation, but sugary foods should be limited.
How should you eat if you have acute pancreatitis?
The diet for acute pancreatitis is as strict as possible: on the menu on the first day there is no food at all, only water. After a few days, you can eat small portions of liquid food - vegetable broths and purees, cooked porridges, mucous broths, liquid meat purees. With approved products you can gradually expand the menu offering.
Diet for chronic pancreatitis
The diet menu for chronic pancreatitis is more diverse, but it is recommended to adhere to it for a longer period, at least six months. It is believed that during this period not only the condition of the pancreas improves, but the patient also weans himself from all sorts of harmful foods, such as fried, smoked and pickled foods.
Traditionally, the "Table No. 5p" diet is prescribed for chronic pancreatitis. The diet table system was developed in the 1920s and, although it has since been abandoned, many doctors still recommend adhering to the principles of such diets.
The "Table No. 5" diet is prescribed for pancreatitis and cholecystitis, but especially for the restoration of the pancreas, a special version of this diet is recommended – "Table No. 5p". It is characterized not only by a reduced fat content in the diet, but also by a limitation of carbohydrates. You need to eat a lot of proteins: Proteins are necessary for the rapid recovery of pancreatic tissue.
The diet for exacerbation of pancreatitis is more strict and is based on the diet recommended for the acute form of the disease. Pureed food, divided meals, avoiding salt and spices will help you cope with the disease faster.
What can you eat if you have pancreatitis (inflammation of the pancreas)?
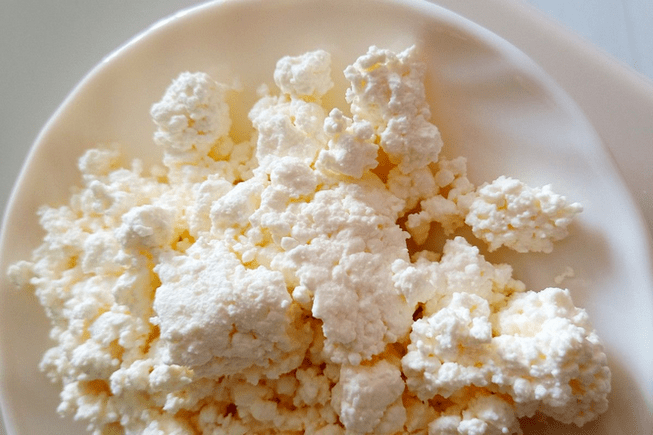
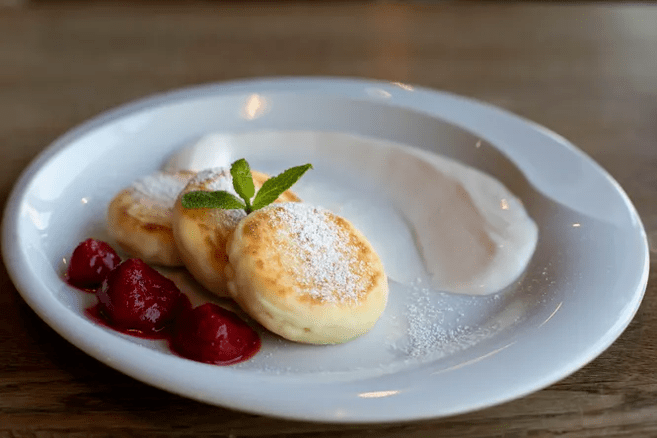
So it's time to find out what you can eat on a pancreatitis diet to recover quickly and avoid painful attacks. We would like to remind you that the list of approved products varies depending on the stage of the disease. During exacerbations, it is recommended to fast and eat a very limited range of foods. However, many more foods are allowed during the remission phase. Low-fat cottage cheese occupies an important place in the diet of people with pancreatitis.
- lean meat (veal, chicken, turkey, rabbit and even lean pork are suitable);
- lean fish (pike, pollock, flounder, cod);
- low-fat cottage cheese, low-fat and mild cheese;
- Eggs in the form of a steamed omelet made from egg whites (you can eat no more than one yolk per day);
- low-fat fermented milk products;
- Milk – only low fat, if tolerated;
- cereals (semolina, rice, oatmeal, buckwheat);
- stale bread, inedible crackers;
- Pasta;
- boiled or baked vegetables (potatoes, beets, carrots, zucchini, pumpkin);
- boiled or baked sweet fruits (apples, bananas, pears);
- Dried fruit;
- Jelly, jam, honey, jelly - in small quantities.
The list of what you can eat on a pancreatitis diet is not so short: if you wish, you can easily do without violations and be content only with permitted foods for a long time. It should be borne in mind that the recommendations were developed 100 years ago and many new products have appeared since then. They can be included in the diet with caution if they are high in protein and low in fat, such as boiled squid.
What not to eat on a pancreatitis diet
The diet for pancreatitis prescribes serious restrictions in the menu, but improvement in the condition can only be expected if it is strictly adhered to. The following foods cannot be included in the diet menu No. 5 for pancreatitis:
- legumes (the only exception is green beans in moderation, boiled or stewed);
- Onions, garlic, radishes, radishes, peppers and other vegetables with a spicy taste;
- spinach, sorrel, fresh herbs;
- all types of cabbage;
- Mushrooms;
- sour fruits;
- marinades and pickles;
- carbonated drinks, packaged juices (it is also better not to drink fresh juices);
- Alcohol;
- coffee and cocoa;
- ready-made sauces, mayonnaise;
- Fast food;
- fresh bread, baked goods;
- all confectionery;
- ice cream;
- fatty meat and fish;
- sausages and delicacies;
- Caviar;
- canned food;
- smoked meat;
- Meat, fish, mushroom broths.
With an exacerbation of pancreatic pancreatitis, the diet becomes even stricter and even foods that can be safely included in the diet during remission can be included in the list of prohibited foods. Here you need to listen to your doctor's recommendations.
Diet for chronic pancreatitis (inflammation of the pancreas): sample menu for a week

We present an approximate diet for a week for chronic pancreatitis. This is not a dogma, but simply a guideline for those who want to restore the pancreas with proper nutrition.
Monday
- Breakfast: a sandwich made from day-old bread with low-fat cheese, a bowl of porridge with water or diluted milk.
- Second breakfast: a portion of low-fat cottage cheese with dried fruits.
- Lunch: Vegetable soup, steamed beef schnitzel with mashed potatoes on water with a small piece of butter.
- Afternoon snack: baked apple.
- Dinner: boiled lean fish, allowed stewed vegetables.
Tuesday
- Breakfast: oatmeal with water
- Second breakfast: baked sweet applesauce
- Lunch: vegetable cream soup, steamed chicken breast; Berry jelly.
- Afternoon snack: low-fat yogurt.
- Dinner: steam omelette with vegetables.
Wednesday
- Breakfast: cottage cheese casserole with dried fruits
- Second breakfast: banana
- Lunch: rice and vegetable soup; steamed rabbit meatballs, compote.
- Afternoon snack: apple jelly, cookies.
- Dinner: stewed fish, vegetable puree.
Thursday
- Breakfast: rice porridge, soft-boiled egg.
- Second breakfast: yogurt, baked apple.
- Lunch: soup with noodles; Fish cakes with vegetable puree.
- Afternoon snack: sandwich with low-fat cheese.
- Dinner: cheese dumplings, a little sour cream.
Friday
- Breakfast: cottage cheese with a spoonful of honey or jam.
- Second breakfast: steamed egg white omelette.
- Lunch: mashed potato soup, baked beef with stewed vegetables, jelly.
- Afternoon snack: dried fruit compote.
- Dinner: lean fish springs, rice.
Saturday
- Breakfast: semolina porridge, soft-boiled egg
- Second breakfast: yogurt.
- Lunch: fish soup with rice, stewed rabbit with potatoes, compote.
- Afternoon snack: cottage cheese casserole.
- Dinner: cheese sandwich, steamed protein omelette.
Sunday
- Breakfast: buckwheat porridge.
- Second breakfast: baked apple.
- Lunch: Pumpkin cream soup, steamed beef chops, noodles.
- Afternoon snack: jelly, cookies.
- Dinner: cottage cheese, boiled vegetables.
Diet for the pancreas: recipes
Despite the limited range of products, the diet for pancreatitis can be quite varied. We offer some ideas for inspiration.

Ingredients:
- rice in bags;
- Potato;
- Carrot;
- Pumpkin;
- Salt.
Preparation: Prepare rice water - cook the rice in a pot with plenty of water, then remove the bags. Grate carrots, chop the remaining vegetables, put everything in a saucepan with rice water, add rice there, cook until the vegetables are ready. Add salt, stir, turn off. If necessary, chop everything in a blender.
Fish quenelles
- Lean fish fillet;
- White crackers;
- Milk;
- Protein;
- Salt.
Preparation: Grind the fish in a meat grinder, soak the crackers in milk, also pass them through a meat grinder, mix with chopped fish. Beat the egg whites until foamy, add to the minced meat, add salt and stir. Form round quenelle from the resulting minced meat. Then boil or steam.
Pumpkin puree soup with oat flakes
Ingredients:
- Pumpkin;
- Potato;
- Hercules;
- Cream;
- Some oil for braising.
Preparation: Cut the pumpkin and potatoes, simmer them in a deep bowl with a little oil, being careful not to burn them. Add salt, add oatmeal, add water, stir, simmer until oatmeal is done. Pass the contents of the pan through a blender, return to the pan, add cream and simmer for a few more minutes. Can be served with breadcrumbs.
According to reviews, it is not entirely easy to follow a diet for pancreatitis, at least in the pureed food phase, but with its help you can achieve a truly stable remission. Patients note that they feel much better on such a diet.
Results of treating chronic pancreatitis with diet
With chronic pancreatitis, the diet is prescribed not for a week or a month, but for at least six months. It is more often recommended to limit yourself to harmful foods for life so as not to provoke an exacerbation.
Together with other treatment methods, a diet for the pancreas has a positive effect on the organ and promotes its rapid recovery. The longer exacerbations do not occur, the more boldly you can expand your diet for pancreatitis, including all new products.
In some cases, thanks to timely treatment and diet, the pancreas is completely restored, and after completing therapy, you can return to your usual nutritional style. Still, it is better to give up unhealthy habits and opt for PP dishes even after full recovery.
The number of different diets cannot be counted. Some of them are prescribed for therapeutic purposes, others are aimed at reducing body weight. A person's diet, like any other organism, affects its health, since the composition of food and its saturation with necessary vitamins and microelements determine the possibility of normal physiology. Any restrictions, both in composition and quantity, inevitably affect our body. Each disease has its own development mechanism and, accordingly, the diet should be different.
The diet for pancreatitis is aimed at reducing inflammation in the pancreas. The sooner you start, the better results you can expect. In the acute stage, fasting can be used, but this usually does not last longer than two to three days. After that, foods with maximum fat restriction are introduced very smoothly. Lean meats and skinless poultry are suitable (veal, lean beef, chicken, rabbit, turkey, etc. ). For garnish you can use buckwheat, barley, mashed potatoes and stewed vegetables. Fried, spicy, salty foods, baked goods, refractory fats (lamb, pork, goose, duck, fatty beef, poultry skin, margarine, mayonnaise) can contribute to a re-exacerbation.
Additional enzyme therapy improves the condition. Preparations made from mini microspheres and microtablets are more effective. The usual dose is about 25, 000 units. The diet described above has its right to exist, however, if its use is justified and it is only adhered to for a short period of time. Stabilization of the condition in pancreatitis is an indication of a planned and gradual expansion of the diet.































